A new study could change the lives of millions of people living with inflammatory bowel diseases (IBD) who don’t respond to the current standard of care.
Researchers at the Kennedy Institute of Rheumatology and Translational Gastroenterology Unit, University of Oxford have identified a potential therapeutic target for IBD. The findings are of particular importance to the 40% of patients who don’t respond to anti-TNF therapy, the current treatment option available.
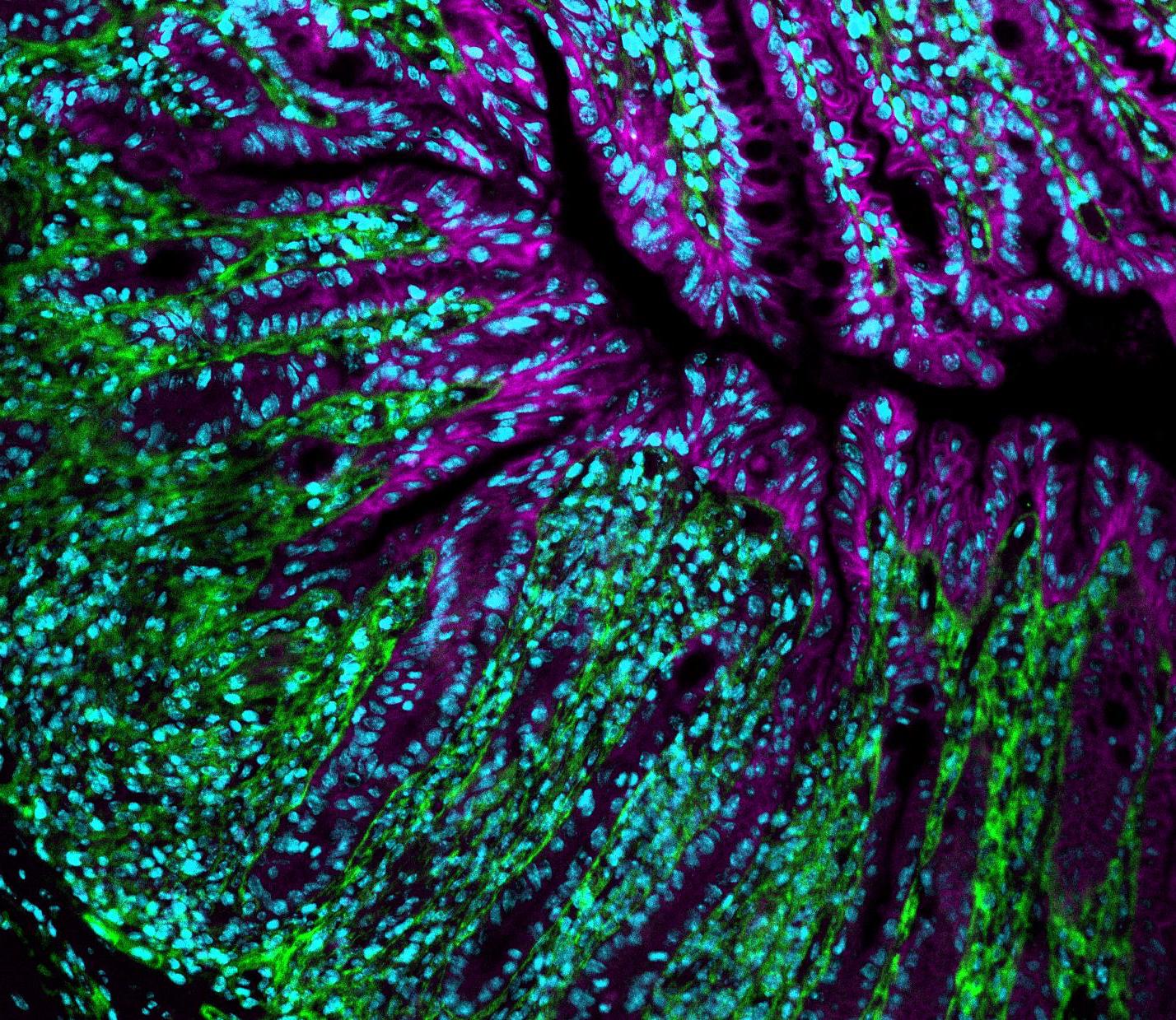
The new study published in Nature Medicine shows that IBD patients have higher concentrations of Oncostatin M (OSM), a protein linked to inflammation, in their intestine and suggest that blocking OSM could prove to be a successful treatment for IBD.
The research also shows that patients with high amounts of OSM in their intestine respond poorly to anti-TNF therapy (such as adalimumab, golimumab, or infliximab), which has been the most effective therapy for IBD for almost 20 years. When tested against samples from a phase 3 trial of anti-TNF therapy, the amount of OSM in gut tissue predicted lack of response.
IBD are chronic painful diseases, which include conditions such as Crohn’s disease and ulcerative colitis. IBD affect at least 5 million people worldwide and this number increases annually, especially in East Asia, although it is most common in Europe and North America.
Director of the Kennedy Institute and lead researcher on the study, Professor Fiona Powrie says: ‘This is a very important finding, because at the moment we are unable to predict which patients will respond well to current therapies; this has an impact on the care we are able to provide to these patients.’
She adds: ‘By understanding more about the immune system in IBD patients we hope to identify markers that allow us to predict which patients will respond to which therapies, ensuring treatments are targeted to those most likely to benefit.’
Genetics plays an important role in IBD, but so do molecules called cytokines that are made by the immune system and regulate the amount of inflammation. Several of these proteins have been considered as treatment targets for patients who don’t respond to anti-TNF therapy, but few have proved effective for treating IBD.
For this study, the research team searched for additional cytokines that could be promoting IBD. Patients were found to have more OSM cytokine in their intestine than healthy controls, with the highest concentrations of OSM predicting which patients would have a poor response to anti-TNF therapy.
This suggests that blocking OSM could prove a successful alternative treatment for IBD and work is underway to test this.
Anti-TNF therapy is expensive and some patients don’t respond well. A test to measure OSM could help target this therapy to patients most likely to benefit.
Professor Powrie said: ‘With around 2 million patients worldwide not responding to the current treatment, it is of paramount importance to find new therapies for IBD. The identification of OSM as a new disease mediator in these patients offers hope for new therapies that can be tested in the clinic.’
Professor Simon Travis, Professor of Clinical Gastroenterology at the University of Oxford and also a co-author confirmed this view: ‘This is really exciting. Until now no one has been able to predict who will or will not respond to anti-TNF therapy. OSM has real potential for selecting the right patient and also as a target for novel therapy to help patients suffering from IBD.’
It is worth noting that OSM is involved in a range of processes to maintain a healthy body, including liver repair and cardiac tissue remodelling. Unfortunately, its over production seems to promote a number of diseases, such as skin and lung inflammation, atherosclerosis, several forms of cancer and possibly arthritis.
The full paper can be read in Nature Medicine.